Ok up until this point we’ve discussed why a spinal fusion is performed and what makes for an ideal spinal fusion. We’ve talked about the importance of minimally-invasive techniques to address pathology without the collateral damage of traditional open midline incisions. We’ve also talked about the importance of large intervertebral spacers to a) achieve fusion, b) restore normal lordosis and c) to achieve indirect decompression of the neural elements. Lastly, we’ve discussed the importance of restoration of lordosis to a) maximize the chances of a good clinical outcome and b) to prevent adjacent segment degeneration. In my opinion, the one technique for lumbar fusion that best achieves all of the above goals is the Extreme Lateral Interbody Fusion (XLIF). First developed in the mid 2000s, this technique allows for the placement of a very large intervertebral spacer at the front of the spine via a small, minimally-invasive incision on the patient’s flank.
We’re going to talk about the specific steps of XLIF in the next post. For now, I’d like to just focus on why I think that XLIF is superior to other fusion techniques. In brief: XLIF is the procedure that allows for the largest possible intervertebral spacer to be inserted via the smallest incision (see figure 1). There are several ways to achieve an interbody fusion of the spine (these procedures have the suffix -IF as in XLIF, ALIF, OLIF, TLIF, PLIF, etc.) These techniques can generally be thought of as either anterior (XLIF, ALIF, OLIF) or posterior (TLIF, PLIF) approaches. Believe it or not, spine surgeons still fiercely debate which way is better. Those in the posterior approach camp say that, through one incision on the patient’s back, they can directly decompress nerves (via laminectomy) and then insert spacers into the disc space and place pedicle screws. Part of the debate here is whether or not a direct decompression of the nerves is even needed. I personally believe that indirect decompression is all you need and you can spare the patient the risk and morbidity of removing bone off of compressed nerves. (I don’t just believe this; I’ve proven it to myself with data from over 300 cases which show that indirect decompression works in greater than 98% of cases.) This is very controversial though and some surgeons aren’t going to be satisfied until they’ve performed a complete bony decompression and have seen the nerves floating free and decompressed.
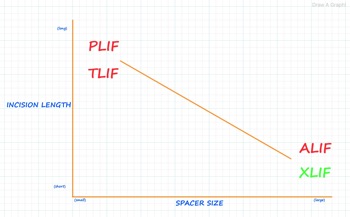
Figure 1: XLIF spacers have the most “bang for the buck” when comparing the size of the spacer with the length of the incision necessary to insert it.
Here’s the problem with posterior approaches though. Remember that the disc space, where intervertebral spacers are placed, is at the front of the spine. In order to place spacers there during posterior fusions the surgeon has to move the thecal sac (fluid-filled sac that contains the nerves) and nerve roots out of the way in order to sneak a spacer around them into the disc space. There’s only so much space to do this so the surgeon really must compromise in terms of the size of the spacer that can be inserted. Thus for TLIF and PLIF the surgeon must insert a very small spacer (see figure 2.) We’ve talked about how important large intervertebral spacers are, the bigger the better in my opinion. The small spacers inserted via TLIF and PLIF can’t contain much graft material to promote bony fusion, aren’t good at restoring lordosis (in fact, some studies show that patients who undergo TLIF and PLIF actually lose lordosis) and lastly, aren’t good at correcting lost disc space and foraminal height. Also, because of where these small spacers sit in the disc space (against the soft bone at the center of the vertebral end plates) they often end up subsiding into the vertebral body above and below (see figure 3). When subsidence occurs the surgeon has failed at achieving one of the main goals of the procedure: restoration of foraminal height and indirect decompression of the neural elements. This failure can lead to recurrence of nerve compression and leg pain resulting in the need for revision surgery with larger spacers.
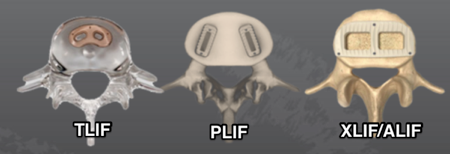
Figure 2: Size matters. Look at the size of an XLIF/ALIF spacer compared to that of the much smaller TLIF or PLIF spacers.
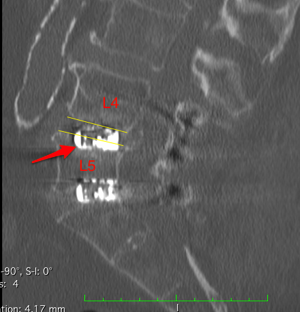
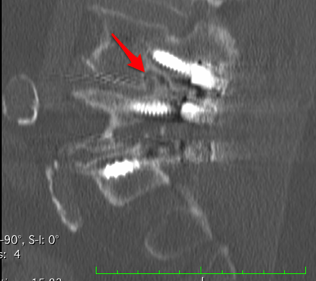
Figure 3: First image shows midline sagittal view of a TLIF spacer (red arrow) subsiding nearly 50% into the endplate of the L5 vertebral body below (the endplates are indicated by the thin yellow lines.) Second image shows severe acquired foraminal stenosis (red arrow) that resulted from the subsidence of the TLIF spacer.
The anterior lumbar interbody fusion (ALIF), in contrast, allows the surgeon to come directly to the front of the spine to insert very large intervertebral spacers without disruption of the posterior elements of the spine. We’ve talked about the benefits of large spacers already so I won’t go into it extensively here. In brief, though, these large spacers are much better at promoting fusion, restoring lordosis and restoring foraminal height for indirect decompression of the neural elements. Think of it from a structural standpoint: would you want your house built on a small/narrow foundation or a large/wide one? The downside to the ALIF, though, is that going through a patient’s abdomen isn’t a benign thing. There are risks of ileus (when the bowels are “stunned” after manipulation during surgery and don’t move for several days. Doesn’t sound like a big deal but it can be an awful complication) as well as injury to abdominal organs or the large blood vessels that sit in front of the spine. Second, the ALIF is usually requires a vascular or general “approach” surgeon who assists in getting the spine surgeon to the spine to do his work. Lastly, if the surgeon does desire to place pedicle screws or do any other work at the back of the spine he’ll have to close up the abdomen and then flip the patient from the supine position (patient laying on their back) to the prone position (patient laying on their abdomen.)
XLIF is just a modified ALIF. Rather than coming through the patient’s abdomen with the patient on their back, the patient is positioned on their side and the surgeon approaches the spine via a small incision on the patient’s flank (see figure 4). You get all of the benefits of a large intervertebral spacer at the front of the spine without the downsides of traditional ALIF. With an XLIF spacer you get a huge graft window to promote robust fusion. Also, because the XLIF spacer sits on the hard bone at the periphery of the vertebral endplates (the apophyseal ring) versus the soft bone at the center of the endplate, it resists subsidence and thus is better at correcting lordosis and foraminal height loss than the smaller TLIF and PLIF spacers (see figure 5). In my opinion there is no question that XLIF is superior to TLIF or PLIF and if I needed a lumbar fusion I’d ask for an XLIF.

Figure 4: Oblique view of ALIF and XLIF trajectories into disc space.
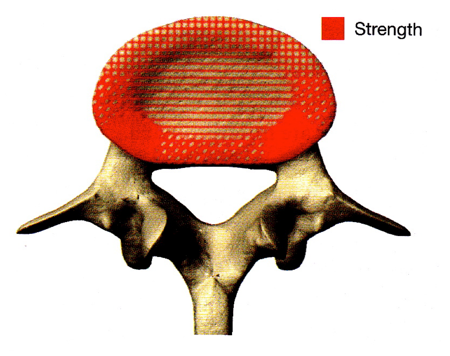
Figure 5: Image showing the stronger, more compact bone at the outer apophyseal ring of the vertebral endplates. XLIF spacers resist subsidence by sitting on the apophyseal ring rather than the softer bone at the center of the endplate. Source: A.A. White, M.M. Panjabi (Eds.), Clinical biomechanics of the spine, 2nd ed, JB Lippincott, Philadelphia, PA, 1990.
If you’ve gotten one of these posterior fusion surgeries don’t email me asking if you got the wrong procedure (you probably don’t need to hear my opinion any more clearly than it’s presented here.) To be fair, there are lots of surgeons out there who routinely perform TLIF and PLIF and do them well. In fact, TLIF is the most common technique for lumbar fusions in the US. These procedures are safe and can be effective. I don’t do them for a reason though. At our hospital we have surgeons who perform every one of these techniques so we have a diverse cohort with which to compare immediate outcomes of these various types of fusion procedures. There’s just something about the immediate structural support and correction afforded by large intervertebral spacers that (again, in my opinion) leads to more rapid and dramatic clinical improvement in patients. One clear difference: my XLIF patients almost always go home the morning after surgery (average length of stay for nearly 200 1- and 2-level cases since 2013 is 1.2 days) while the TLIF and PLIF patients of other surgeons stay in the hospital at least twice as long if not longer. If you include training, I’ve been doing the XLIF procedure since 2006 and the clinical outcomes afforded by this technique still amaze me to this day.
So if XLIF is so great why doesn’t every spine surgeon do XLIF and only XLIF for their lumbar fusions? The answer is that there are some perceived limitations of XLIF that scare some surgeons into not doing this procedure:
- Surgeons think that after XLIF you have to close up and then flip the patient prone to place screws (similar to the real limitation described for ALIF.)
- Because the iliac crest of the pelvis gets in the way, XLIF can’t be done at L5/S1 (ok, this is a real limitation, not a perceived one.) So if a surgeon is fusing L4/5 and L5/S1 (which is required quite often actually) you’ll have reposition the patient from the lateral position to some other position to fuse L5/S1 using a different technique.
- XLIF has an unacceptably high risk of nerve injury, especially when done at L4/5.
Over the next few posts I’ll discuss why these are just perceived limitations of XLIF. In fact, XLIF is a very safe and effective way to perform a lumbar fusion, even at the L4/5 level (greater than 95% of the lumbar fusions that I do involve XLIF at the L4/5 level.) Also, when XLIF is combined with Lateral ALIF (a minimally-invasive ALIF done with the patient on their side) at L5/S1 and single-position pedicle screw fixation (pedicle screws placed with the patient in the lateral position without flipping prone) a surgeon can perform a robust lumbar fusion from L1 to the sacrum without repositioning the patient. This strategy of Lateral Single Position Surgery (LSPS) dramatically reduces the anesthesia time for patients, which translates into decreases risk and improves outcomes. More on this ground-breaking concept in future posts.
Thanks for reading!
J. Alex Thomas, M.D.

Very nice summary of XLIF,
Having had a successful L4-S1 TOPS hardware installation in London almost a decade ago to solve a Cauda Equina issue, L3-L4 decompression a couple of years ago and looking at a planning strategy for some scoliosis and severe L2-L3 stenosis, my appreciation for the clarity of expression, deft and competent exposition of a subject of rather pressing interest.
It is astonishing how rare it is to find high value information these days. I look forward to reading your material further.
This blog really helped me to understand the procedure more then I did by just reading. The fact that it was in your words and expressed the knowledge surrounding your opinions meant a lot. Still nervous but feel this is the best route for me. Appreciate your candor.