We talk a lot at Spinal (con)Fusion about different painful conditions of the spine and their treatments. It occurred to me, though, that I haven’t spent much time talking about pain specifically. How is it perceived? Why does the brain perceive it in such a way? How can these perceptions be altered or attenuated? It turns out that the answers to these questions lie deep within that which makes us human: our brain. It turns out that your pain is all in your head.
Pain is modulated by several different regions in your brain. How do we know this? In the past, we’d have to rely on animal models in which scientists would injure part of the animal’s brain and then study the effects of that injury. Over the past decade or so, however, we now have a non-invasive way to study the function of the brain: functional MRI or fMRI. This is a unique form of MRI imaging that looks at differences in blood flow in certain brain regions when a patient performs a task or is in a specific physiologic state. Over the past 10 years in particular, fMRI (and large AI-driven databases of established fMRI data) has unlocked a new world of understanding about the regions of the central nervous system that process acute and chronic pain. What have we learned?
When you, say, touch a hot stove, the painful stimulus is transmitted from special sensors in your fingertips via unmyelinated (uninsulated) C-type nerve fibers (I only mention this specifically because this type of fiber is well preserved over hundreds of millions of years of evolution because even the most basic primitive creature had to be able to perceive pain from the periphery and avoid it.) The pain signal then enters the gray matter of the spinal cord, crosses over to the other side of the spinal cord and ascends via the spinothalamic tracts to the brain (hence, if you touch a hot stove with your left hand you’re perceiving it in your right brain.) It takes about 100 milliseconds for this signal to travel from your hand to the brain. The thalamus is the first stop within the brain for information on painful stimuli transmitted from the periphery. These signals are analyzed within the thalamus and then transmitted to the primary sensory cortex at the surface of the brain (this part of the brain is somatotopically organized meaning that each part of the body is represented in different zones of the sensory cortex, see figure 1.) The primary sensory cortex (along with the posterior insular cortex) are then able to analyze the nature and intensity of the painful stimulus–basically, these regions collect and analyze the basic facts about the pain, the “what, where and how bad” of the pain.
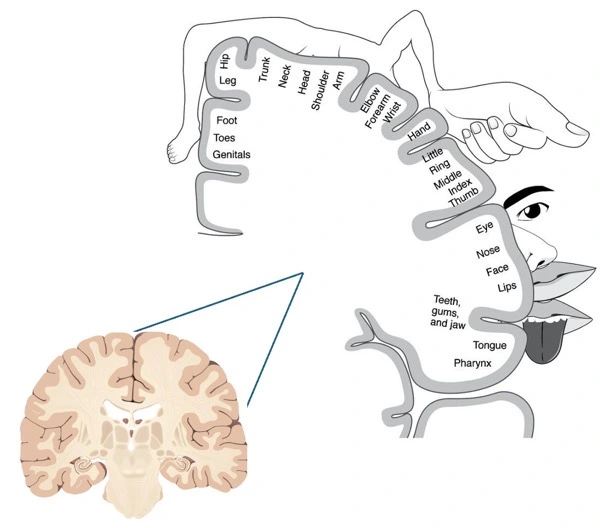
Figure 1: the sensory homonculus demonstrating the somatotopic organization of the primary sensory cortex. Source, in part: Baweja, 2020.
Ok, so back to the hot stove. Of course, you know that the stove is very hot, and you know which appendage on which side of your body is in contact with the stove (e.g. “OUCH!! My left hand is burning!”) This is all the work of the spinothalamic tract, the thalamus and lastly the primary sensory cortex. From there it gets much more complicated. From the sensory cortex a number of projections extend out to other brain regions which analyze the pain on a much deeper level (see figure 2.) First, there are projections to the secondary sensory cortex and anterior insular cortex that allow to the brain to assign a degree of context and unpleasantness to the stimulus (e.g. “OUCH! My left hand is burning and it’s awful and it could be because I wasn’t paying attention to where my left hand was when I was scrolling on my phone with my right hand!”). Next (and these projections out of the primary sensory cortex are all happening concurrently), there will be projections to the primary and supplemental motor regions to immediately to move your arm to escape the pain and to plan avoidance strategies to prevent burning yourself again (e.g. “OUCH! My left hand is burning! I’m gonna pull my left hand back RIGHT NOW, oh and next time I’ll put my left hand in my pocket when I’m scrolling on my phone with my right hand.”) There will also be projections to prefrontal cortical regions such as the anterior cingulate cortex and dorsolateral cortex which are involved in higher cognitive processing about the pain (e.g. “OUCH! My left hand is burning…and MAN…that hurts! But it this pain really a threat to me? Maybe it’s not really harming me, and I shouldn’t freak out?”). There are also direct projections from the thalamus to the rostral dorsal anterior cingulate cortex (rdACC) and anterior insular cortex that modulate that extent of emotion and suffering attributed to the painful stimulus (e.g. “OUCH! My left hand is burning and I this is really hard on me…I’m really suffering here and don’t know if I could ever endure something like this again.”) Lastly, there are projections to the amygdala and hippocampus regions that also somewhat modulate fear and emotional responses to the pain but also the imprinting of memories about the pain and its context (e.g. “OUCH! My left hand is burning! This has been a scary experience. I’m going to remember this and probably will never go near a stove again.”) Some researchers have boiled down these pathways into a lateral system which process the details of the painful stimulus (i.e. the “painfulness” component), and a medial system which processes the cognitive and emotional responses to the painful stimulus (i.e. the suffering component, De Ridder et al 2021). Importantly, in addition to these ascending pathways, there is a set of descending pathways that can suppress the pain information coming into the brain. These pathways allow you to identify and adapt to sources of pain so that they don’t become too disruptive. These descending pathways are especially influenced by the context under which the pain was experienced; for example, these pathways become more active when pain is perceived as pleasurable as in the burn of an intense workout (see figure 3.) These three groups of pathways, all confirmed by large fMRI studies, are kept in a finely tuned homeostasis via connections that run through the thalamus.

Figure 2: Brain regions for perception of pain.
This all may seem excessively complicated but put simply, there is a so-called “neuro-matrix” of different regions the brain that regulate many different aspects of one’s perception of pain. While these connections are similar between all people, some of the connections may be more impactful than others from one person to the next. For example, an elite ultra-marathoner who has learned not only to manage pain but perhaps even to embrace it is going to have much different wiring of these pathways than, say, a couch potato to whom the thought of running to even the mailbox elicits pain and anxiety. Of course, there are likely genetic differences between people that can predispose them to these differences in their pain pathways. Generally speaking, however, it’s helpful to think that at least early on in life these pathways are similar between people but then are remodeled over a person’s life based on their life context and experiences with pain (more below.) These pathways can change, because just like about all the other wiring in the brain, the neuronal pathways of pain have a high degree of plasticity. In other words, they can change, for better or worse.

Figure 3: This guy’s descending (inhibitory) pain pathways are on overdrive! Source: https://www.nytimes.com/2011/05/03/science/03firewalker.html
The normal anatomical “wiring” of pain perception that we’ve discussed up until this point can generally be thought of as relating to the perception of an acute, short-lived process like a painful radiculopathy or the mechanical back pain of a mobile spondylolisthesis. But what happens in chronic pain (a.k.a. pain that persists 3-6 months after a radiculopathy/episode of back pain should have healed)? Here, the pain truly is in the brain.
Many factors can lead to a patient transitioning from acute to chronic pain. It’s generally thought that repetitive pain leads to a localized increase in neuro-inflammatory markers which then leads to peripheral and the central sensitization. Basically, the brain gets used to the pain and begins to expect it and even perceive it in the absence of a painful stimulus. The patient develops a hypersensitivity to even the slightest of pain and thus begins to chronically perceive pain. This transition doesn’t happen in everyone though; certain people are more susceptible to the development of chronic pain than others. First, as we mentioned, genetic variations in the expression of certain inflammatory markers or neurotransmitters can make someone more likely to develop chronic pain. Second, epigenetic factors may also come into play (i.e. how your environment alters the expression of your genes): traumatic/stressful events in childhood, low socio-economic status, environmental toxins and poor diet have all been linked to this transition. Lastly, recent research suggests that even the gut microbiome may play a significant role in predisposing patients to the transition from acute to chronic pain. There essentially is a direct connection between the gut and the central nervous system that modulates one’s inflammatory response and thus can then affect peripheral and central sensitization to pain. Finally, when central sensitization occurs in the setting of preexisting psychological disorders such as depression and anxiety the conditions are ripe for the development of the chronic pain. Now, the medial pathways that encode the suffering response to pain become overly active and the inhibitory pathways become attenuated or even completely absent. Fear, anger and anxiety take over. With time, measurable structural alterations occur in the brains of patients with chronic pain. Patients with chronic pain get loss of neurons in regions of the brain that help modulate and critically assess pain, making them less resilient when dealing with pain in the future. So, patients with chronic pain aren’t crazy or weak in the face of pain; no, their brains physically change in the setting of chronic pain.
In closing, fMRI studies have clearly shown that patients with chronic pain have definitive structural changes to their central nervous system. These changes cause the “suffering” component of the pain, the fear and anxiety of the pain, to be amplified and can cause the patient to experience severe pain, even in the absence of ongoing painful stimulus. In short…patients become wired for chronic pain. Here’s the good news though: plasticity goes both ways. The rewiring and structural changes seen in the brains of patients with chronic pain can be modulated and even reversed. In our next post we’ll talk about various therapies that reverse these structural changes to treat chronic pain.
Thanks for reading!
J. Alex Thomas, M.D.
References:
Baweja, Akshay. (2020). Haptic Glove Display: Enabling Sensory Substitution. International Journal of Scientific & Technology Research. 9. 4759 – 4763.
De Ridder D, Adhia D, Vanneste S. The anatomy of pain and suffering in the brain and its clinical implications. Neurosci Biobehav Rev. 2021 Nov;130:125-146.

Hello again Dr. Thomas! I found your latest post to be fascinating, ‘con’fusing, and stimulating all at the same time. As someone who is more than two years from spine surgery, I don’t experience any chronic pain. However, when over-extending myself in the garden, or playing with my puppy, bending at the waist always causes me a great deal of pain. This is not the same pain I experienced pre-surgery. I have self-diagnosed it as a result of the pins in my spine and try to limit bending. Of course not bending is next to impossible for an active person like me! I do wonder now if this is a brain reaction as you describe here, or is it an actual result of pain caused by bending at the waist. I’m interested to see what more of your readers have to say about this! So nice to hear from you again. Best wishes, June
June Sweeny 221 Beech St. Wilmington NC 28405 (910) 617-7687